Shoulder Surgery Rehabilitation at Home
Recovering from shoulder surgery is a unique challenge. Unlike lower limb surgeries where mobility is the primary hurdle, shoulder procedures—such as rotator cuff repairs, stabilisations, or total shoulder replacements—often require you to navigate daily life with the use of only one arm for several weeks.
This period of immobilisation, combined with the need to protect the surgical repair, makes the home environment the most logical place for rehabilitation. You are not just recovering movement; you are relearning how to dress, sleep, and wash safely within your own space.
At Medella, we bring rehabilitation to you. By combining Chartered Physiotherapy with Occupational Therapy, we support both the clinical healing of your shoulder and the practical adaptations needed to maintain your independence during recovery.
Understanding Shoulder Surgery Recovery
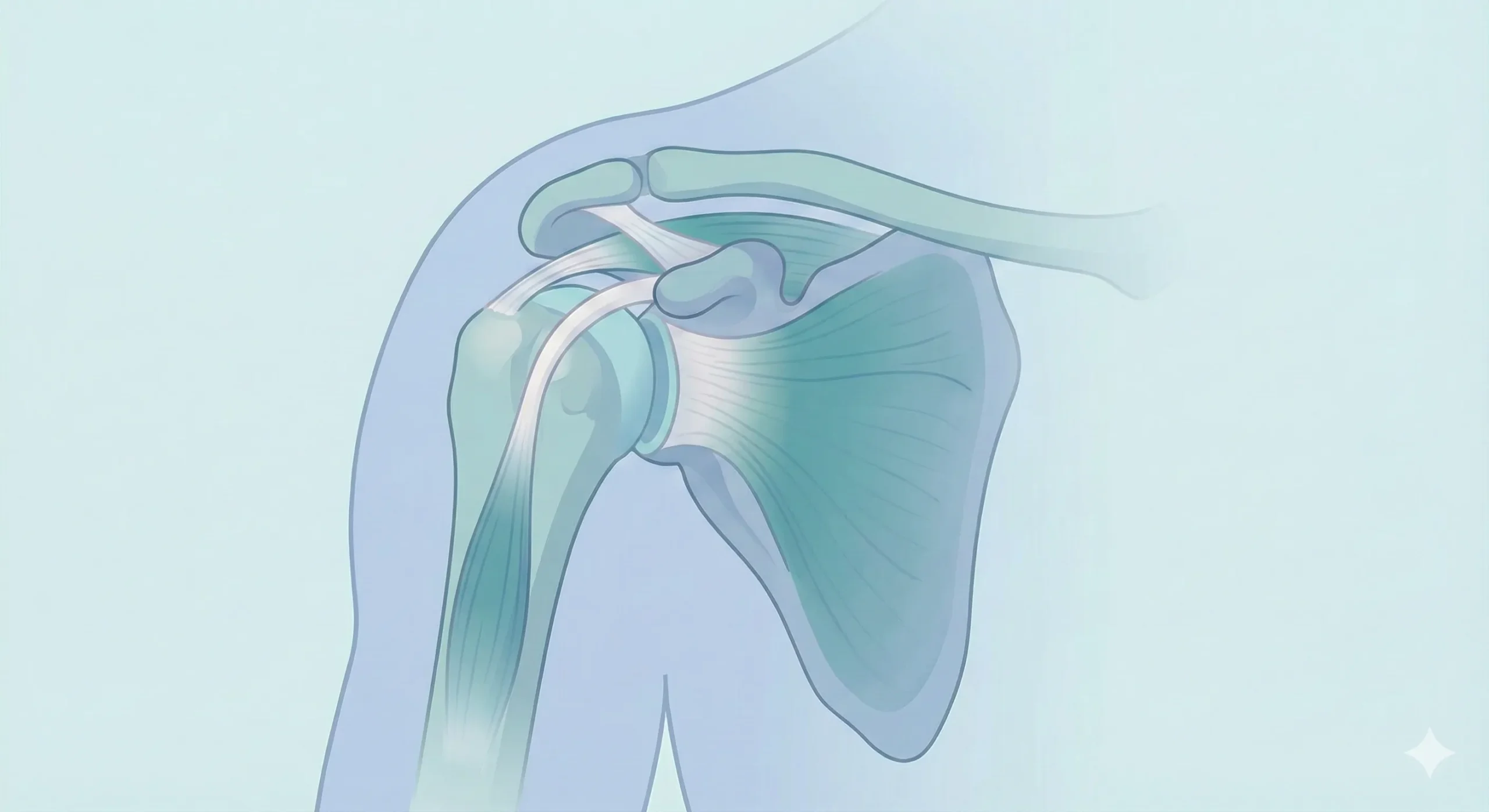
Shoulder surgery is a major intervention designed to restore function or stability to the complex ball-and-socket joint. Whether you have undergone a planned elective procedure or emergency surgery following trauma, the early days are defined by a delicate balance: protecting the repair while preventing secondary stiffness.
The impact on your daily life is immediate. With your arm likely in a sling or immobiliser, balance can feel altered, and simple tasks like preparing a meal or getting comfortable in bed become significant logistical challenges. Understanding that this frustration is a normal part of the process is the first step in recovery.
Common Procedures We Treat
- Rotator Cuff Repair: Reattaching torn tendons to the humeral head.
- Total Shoulder Replacement: Replacing damaged joint surfaces with prosthetic components.
- Subacromial Decompression: Increasing space in the shoulder to prevent impingement.
- Stabilisation Surgery: Tightening ligaments or repairing the labrum after dislocations.
- Fracture Fixation: Surgical plating or pinning following a break.
Was your surgery the result of a fall? We can also integrate falls prevention strategies into your rehab plan.
Phase 1: Protection
Focus: Immobilisation & Passive Movement.
In the initial weeks, the priority is protecting the surgical site. Your arm will likely be in a sling. Our focus is on pain management, wound care, and maintaining movement in your elbow, wrist, and hand to prevent stiffness elsewhere. We may perform very gentle passive movements of the shoulder strictly within the surgeon's protocol.
Phase 2: Activation
Focus: Assisted Active Movement.
As tissues heal, we wean off the sling. We introduce "active-assisted" exercises where you begin to move the arm using your own muscles, often supported by your therapist or a pulley system. The goal is to restore range of motion without overloading the healing tendons.
Phase 3: Strengthening
Focus: Function & Control.
Once range of motion is satisfactory, we build load tolerance. This involves strengthening the rotator cuff and scapular (shoulder blade) stabilisers. Rehabilitation shifts toward functional tasks—reaching, lifting, and returning to hobbies or work duties.
Common Difficulties During Recovery
It is helpful to anticipate the specific hurdles associated with shoulder rehabilitation so you can prepare your home environment. The most frequent challenges our patients report include:
- Sleep Disruption: Finding a comfortable position while wearing a sling or dealing with post-operative aches is notoriously difficult. Lying flat is often uncomfortable.
- One-Handed Hygiene: Washing hair, fastening buttons, or simply drying off after a shower requires new techniques.
- Fear of Movement: After a painful injury or surgery, it is natural to feel anxious about moving the arm again. This "guarding" behaviour can inadvertently lead to a frozen shoulder if not managed gently.
- Neck and Back Strain: Wearing a sling alters your posture, often causing compensatory pain in the neck and upper back.
How Physiotherapy Supports You
Our Physiotherapists focus on the mechanics of the joint and the healing of soft tissues. During home visits, we provide:
- Passive Mobilisation: We gently move the joint for you in the early stages to maintain range without stressing the repair.
- Scapular Control: The shoulder blade is the foundation of shoulder movement. We teach you how to set and control the scapula to prevent impingement.
- Soft Tissue Release: Manual therapy to release tight muscles in the neck and chest that often seize up from sling wear.
- Safe Progression: We guide you precisely on when to push for more movement and when to rest, adhering strictly to your consultant’s restrictions.
How Occupational Therapy Supports You
Our Occupational Therapists focus on the "doing" aspect of recovery. We ensure you can function safely at home while one-handed:
- One-Handed Strategies: Practical techniques for dressing (how to put a shirt on the operated arm first), grooming, and food preparation.
- Sling Management: Coaching on how to don and doff your sling safely without breaching movement precautions.
- Home Adaptations: Recommending temporary aids—such as shower stools or pump-dispenser bottles—to reduce fatigue and fall risks.
- Energy Conservation: Everything takes longer with one arm. We help you pace your day to manage fatigue.
Sleeping Positions
Many patients find it impossible to sleep flat initially. We often recommend propping yourself up in a semi-reclined position using a V-shaped pillow, or sleeping in a recliner chair for the first few nights to reduce throb.
Dressing Tips
Wear loose, button-up shirts or cardigans rather than pullovers. Always dress your operated arm first and undress it last. This minimizes the need to reach or rotate the shoulder.
Kitchen Safety
Avoid lifting heavy kettles. We recommend using a kettle tipper or filling a thermos flask in the morning so you have access to hot water throughout the day without repeated lifting.
How Home Visits Work
Our service begins with a comprehensive assessment in your home. We serve patients across Hampshire, Dorset, and Wiltshire, bringing hospital-level care to your doorstep.
We review your discharge letters and operation notes to understand the exact nature of your surgery. Because our team has an average of 18 years of experience, we can assess you in the exact chair you sit in and the bed you sleep in, providing advice that is tailored to your reality, not a clinical simulation.
Sessions typically last 45 minutes to an hour. Your therapist will bring all necessary equipment, including bands, weights, and treatment tables if manual therapy is required.
⚠️ Red Flags: When to Seek Advice
While recovery has its ups and downs, you should contact your medical team or GP immediately if you experience:
- Signs of infection (redness, heat, swelling, or oozing at the wound site).
- A sudden, sharp pain accompanied by a "pop."
- Loss of sensation or persistent coldness in the hand or fingers.
- Shortness of breath or calf pain (potential signs of clotting).
Shoulder Rehabilitation Experts
Shoulder recovery requires a careful, expert touch. Our senior therapists help you restore function and movement safely at home. View full team profiles →
Frequently Asked Questions
When can I drive after shoulder surgery?
You generally cannot drive while wearing a sling. Most patients return to driving between 6 to 12 weeks post-surgery, but this is strictly dependent on your surgeon's approval and your ability to control the vehicle safely during an emergency stop. You must notify your insurance provider.
How long will I need physiotherapy?
Shoulder rehabilitation is a marathon, not a sprint. While soft tissue healing takes 6–12 weeks, full strength and range of motion can take 6–12 months to return fully. Our involvement scales down as you become more independent with your exercise programme.
Do I need a referral?
No, you do not need a GP referral to access our private home physiotherapy or OT services. We can begin working with you as soon as you are discharged from the hospital.
Unsure if home rehab is right for you?
We don't use call centres. Speak directly to our Clinical Director, Naomi, for free, professional advice on your recovery options.

















