
If you have ever mentioned a stiff knee or an aching hip to a friend and been told, "Well, it’s just your age," you are certainly not alone. It is one of the most common phrases heard by people over 50—and unfortunately, one of the most unhelpful.
While it is true that our bodies change as we get older, dismissing pain as an inevitable consequence of ageing can leave you suffering needlessly. The belief that you must simply "put up with" discomfort can lead to a gradual loss of independence, as you may start avoiding the activities that keep you healthy and happy.
The good news is that joint pain—even when caused by arthritis—is not something you have to endure in silence. Modern evidence shows that with the right management, you can reduce pain, improve your mobility, and continue doing the things you love.
The Reality of Joint Pain in Older Adults
Joint pain is undeniably common. Approximately one in five adults over 45 in England have osteoarthritis of the knee, and one in nine has it in the hip. So, if you are experiencing stiffness or discomfort, you are certainly not imagining it.
However, "common" does not mean "untreatable". Osteoarthritis (OA) is often described as "wear and tear", where the cartilage cushioning your joints gradually changes. While this sounds alarming, it is a process that can be managed effectively. It is distinct from Rheumatoid Arthritis (RA), which is an autoimmune condition requiring different medical management.

Crucially, an X-ray showing changes to your joints does not always equal pain. Many people have significant "wear" on scans but experience very little discomfort. This proves that pain is not just about the structure of your bones—it is about how strong, mobile, and supported those joints are.
Why "Just Resting" Is Often the Wrong Approach
When a joint hurts, our natural instinct is to protect it. You might decide to skip your morning walk, avoid the stairs, or stop gardening. It feels intuitive: if it hurts to move, surely you should rest?
Unfortunately, too much rest can create a vicious cycle:
- Reduced Movement: You move less to avoid pain.
- Muscle Weakness: The muscles supporting your joint become weaker.
- Increased Strain: With less muscular support, the joint takes more load, leading to more pain.
- Deconditioning: You lose confidence and independence.
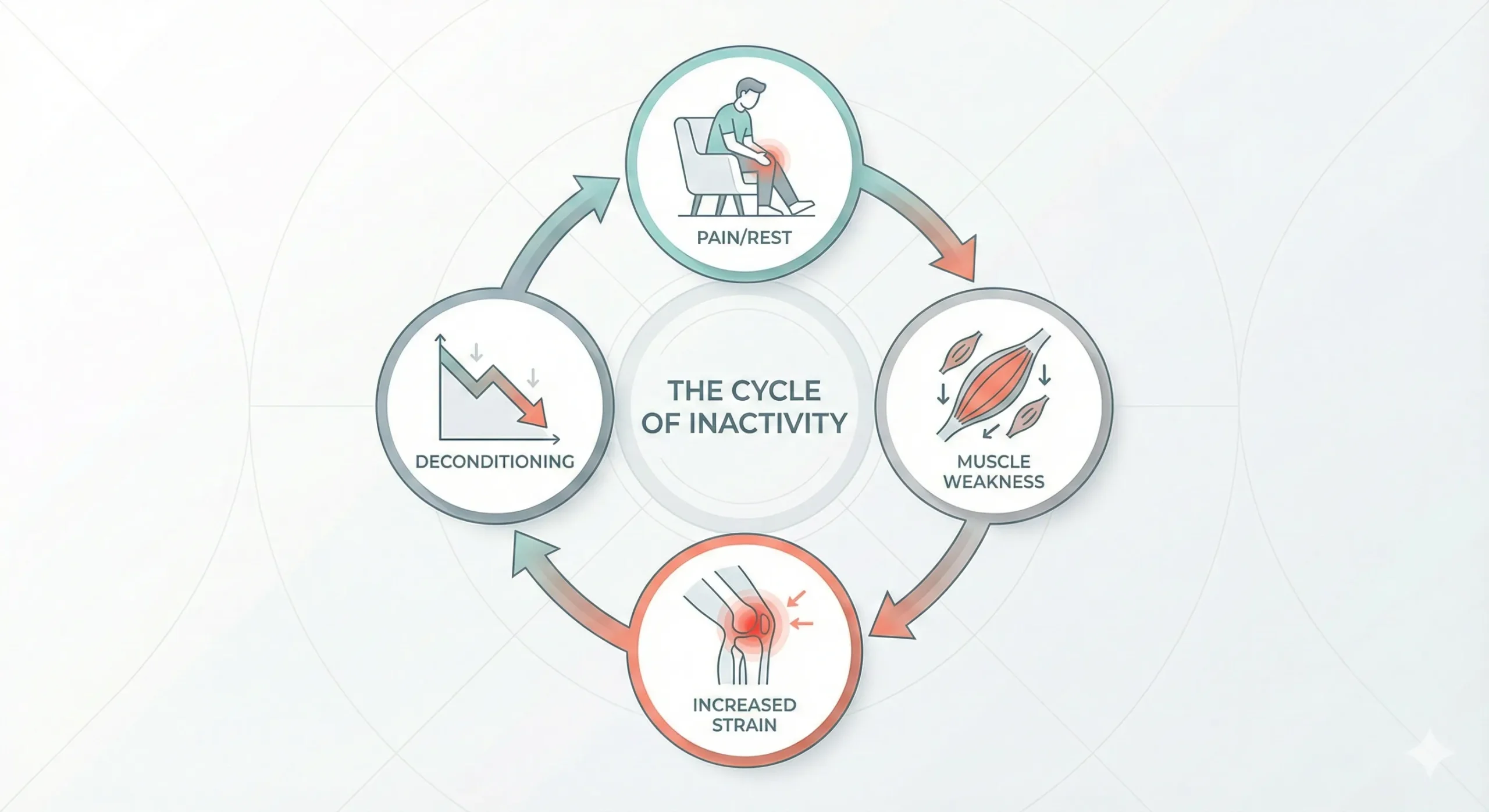
Breaking this cycle is the key to feeling better. Joints rely on movement to circulate fluid and nutrients. As the saying goes in physiotherapy: "Motion is lotion."
Movement is Medicine: How Physiotherapy Helps
The National Institute for Health and Care Excellence (NICE) guidelines are clear: the core treatments for osteoarthritis are therapeutic exercise and weight management. This is where specialised physiotherapy for arthritis becomes invaluable.
You do not need to train for a marathon to see benefits. Gentle, consistent movement—such as walking, cycling, or swimming—can strengthen the muscles around your joints, taking the pressure off the bone itself.
A physiotherapist can help you by:
- Assessing your movement: Identifying exactly which muscles are weak or tight.
- Creating a tailored plan: Prescribing safe exercises that build strength without flaring up your pain.
- Building confidence: Helping you understand what "safe pain" feels like so you are not afraid to move.
Practical Ways to Protect Your Joints
Managing arthritis is not just about exercise; it is also about how you use your body throughout the day. This is often where Occupational Therapy (OT) complements physiotherapy perfectly.

Small changes to your daily routine, known as "joint protection principles", can make a significant difference:
- Pace yourself: Break larger tasks (like cleaning or gardening) into smaller chunks with rests in between.
- Use your strongest joints: For example, carry a shopping bag on your forearm or shoulder rather than gripping it tightly with your fingers (as illustrated).
- Avoid staying in one position: If you are sitting or standing for a long time, gently move or stretch every 20 minutes to prevent stiffness setting in.
If daily tasks are becoming difficult, home adaptations or simple aids can also help reduce the strain on your joints, keeping you independent at home.
When to Seek Professional Help
While some aches are normal, you should seek advice if:
- Pain is disturbing your sleep or affecting your mood.
- You are noticing a loss of balance or feel unsteady on your feet.
- You have had a fall, or are worried about falling.
- Your joint is hot, red, or swollen (this requires urgent medical attention).
Frequently Asked Questions
Is joint pain always caused by arthritis?
Not always. Joint pain can be caused by bursitis, tendonitis, or simple muscle strain. However, persistent stiffness (especially in the morning) is a common sign of osteoarthritis. A proper assessment can clarify the cause.
Will exercise make my arthritis worse?
No, appropriate exercise is actually protective. While you should avoid high-impact activities during a painful "flare-up," keeping the joint moving is essential for long-term health. A physiotherapist can guide you on the right level of activity.
Can physiotherapy help if I am already on a waiting list for surgery?
Absolutely. "Pre-habilitation" (getting fit before surgery) is highly recommended. Stronger muscles often lead to a faster recovery after a hip or knee replacement.
You Don't Have to Accept Pain
The most important message to take away is that you have options. Joint pain is not a life sentence, and it is certainly not something you have to accept just because of the year on your birth certificate.
By staying active, pacing your activities, and seeking the right professional support, you can protect your joints and protect your quality of life.
